MEDITWIN: using digital twins to develop tomorrow's personalized medicine
MEDITWIN: using digital twins to develop tomorrow’s personalized medicine
How can the use of virtual twins improve the quality of care, making healthcare safer and more accessible for all? This is the mission of MEDITWIN, a consortium of 7 Instituts Hospitalo-Universitaires (IHUs) including IHU ICAN, from Nantes University Hospital, Inria, associated startups and Dassault Systèmes, announced on Monday, December 11, 2023 in the presence of French President Emmanuel Macron..
Thanks to personalized virtual twins of organs, metabolism and cancerous tumors, this innovative project will make it possible to diagnose the risk of cardiovascular disease for high-risk patients, and to help specialized physicians choose treatments for effective patient follow-up.
The MEDITWIN initiative will be developed over 5 years, from 2024 to 2029. The partners’ investment in this project will be financially supported by the French government as part of France 2030.

What medical need does MEDITWIN meet?
“Digital twins open up the prospect of a new form of precision and preventive medicine for cardiometabolic diseases, by establishing for each individual his or her future risk of developing cardiovascular disease, based on risk factors such as his or her genomic signature. Such a project requires a change of scale in research, which has now been achieved thanks to the project led by Dassault Systèmes, with all the MEDITWIN partners on board.”
Prof. Stéphane Hatem, General Director of the ICAN IHU and Director of UMR 1166 Cardiovascular and Metabolic Diseases

Cardiometabolic diseases, also known as cardiovascular-metabolic diseases, refer to a group of interconnected disorders affecting the heart and metabolic system. They mainly include: cardiovascular diseases affecting the heart and blood vessels (coronary heart disease, hypertension…) and metabolic disorders (type 2 diabetes, obesity, hypercholesterolemia, steatotic liver disease – MASH-(NASH)).
Cardiovascular disease is the world’s leading cause of death, accounting for almost 18 million deaths every year. In France, they represent the 2nd cause of death in the general population, with almost 150,000 deaths each year, and the 1st cause in women. More than 15 million people are treated in France for disease, cardiovascular risk or diabetes, at an annual cost of over 17 billion euros.
To date, all symptomatic and asymptomatic patients at risk are assessed for cardiovascular risk by their physicians.
The association between certain classic biological markers (classic lipid profile, LDL-cholesterol) and the risk of cardiovascular disease is indisputable. However, to date, the use of these markers in medical practice does not allow for fine stratification of this population.
Without predictive tools, it is difficult to individualize patient follow-up and choose the most appropriate treatments and optimal doses, while reducing the side effects associated with treatment (statins).
Technical advances not yet systematized
Scientific and biomedical research has made significant advances in this field, with plans to integrate other markers based on imaging and Omics data (metagenomics, metabolomics, lipidomics, proteomics).
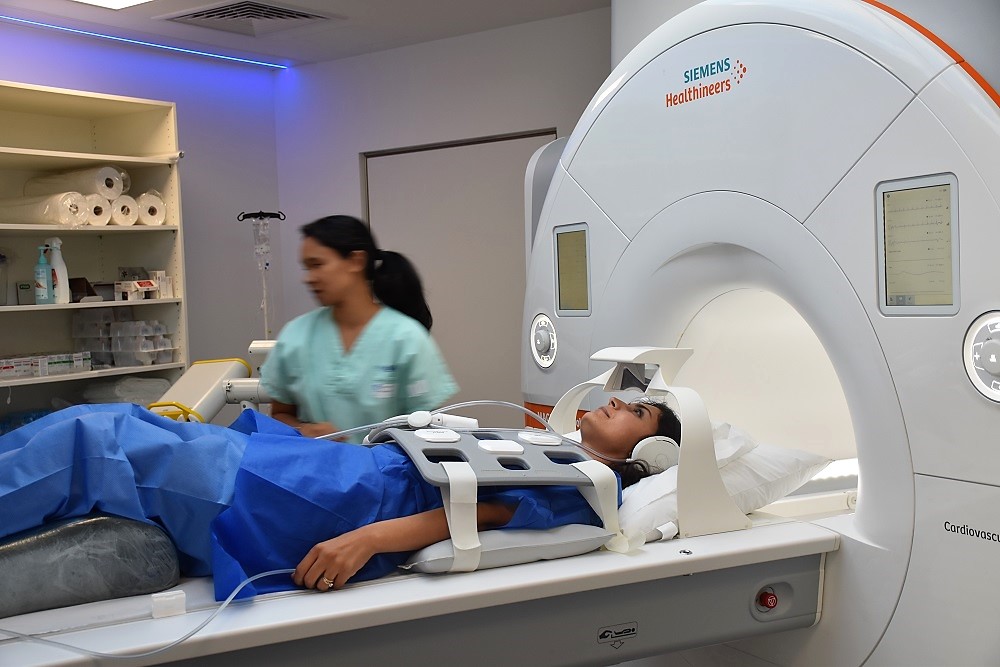
Advances in imaging techniques, such as thoracic CT scans (large and small arteries), now enable non-invasive, detailed analysis of vascular damage in patients with no known cardiovascular disease.
By revealing the progression, stabilization or regression of the disease and predicting the quality of response to treatment, these new indicators become a concrete means of applying prevention and targeted therapies according to the patient’s profile and biology.

Familial hypercholesterolemia (FH) is a major cause of premature cardiovascular disease, and represents a model of accelerated pathological progression. Following the trajectory of these patients is therefore an opportunity to access risk prediction indicators within a limited timeframe.
Recent data have shown that, even in the case of familial hypercholesterolemia, the use of non-invasive coronary imaging can predict the incidence of cardiovascular events in asymptomatic subjects, with high predictive power over a follow-up of less than 3 years.
However, these techniques are not fully integrated into decision-making algorithms, and their use in clinical practice is not systematized.
Using virtual twins for a better treatment strategy

With this use case for virtual twins, the MEDITWIN consortium’s ambition is to develop a personalized predisposition diagnostic service for cardiovascular disease, and to select the best treatment strategies, while integrating the patient’s environment, such as gut microbiota and nutrition.
The predictions of such twins in terms of trajectories and their improvement could support the practitioner in the management of the patient, and also make more tangible the patient’s future in the absence of intervention in order to improve adherence to treatment. This will make it possible to measure the impact of proposed solutions in terms of reducing the number of patients with cardiovascular events (coronary, cerebrovascular, arterial…).
The benefits will be felt by patients, who will benefit from care tailored to their individual risk and directly linked to the progress of their disease, and by practitioners, who will be able to take advantage of tools for the early identification and management of chronic diseases.
MEDITWIN will therefore enable a digital twin model to be established to monitor the individualized cardiovascular risk of patients with familial hypercholesterolemia, thanks to a selection of relevant biomarkers.
Digital twins will help to clarify the cause-and-effect relationship between micro and macro-circulation in a healthy cardiovascular system, so that we can better understand the pathophysiological mechanisms of aging, hypertension, diabetes and other conditions.
Heart failure: the UTHop'IA project reinforces therapeutic education during hospitalization
Heart failure: the UTHop’IA project reinforces therapeutic education during hospitalization
Heart failure is a chronic disease that requires lifelong monitoring. As with all chronic diseases, therapeutic education plays a major role in the management of the disease, by involving patients and their families in the care process. It means better compliance with treatment, fewer hospitalizations and a better quality of life.
Led by IHU ICAN, the UTHop’IA project aims to support heart failure patients from hospitalization to their return home, using digital tools and artificial intelligence.
Find out more about the 5 projects included in UTHop’IA, involving CapGemini and students from the ECE engineering school, Polytech and Pantheon-Sorbonne University.

What medical problems does the UTHop’IA project address?
Heart failure affects around 1 million people in France, and 120,000 new cases are diagnosed every year. This chronic disease is responsible for 200,000 hospitalizations and 70,000 deaths every year. It mainly affects people over the age of 75, but can also affect much younger people. Malgré les progrès de la prise en charge, un patient sur deux meurt dans les cinq ans suivant le diagnostic.

Since 2006, doctors in the cardiology department at Hôpital de la Pitié-Salpêtrière have been running a therapeutic education program (ETP) for heart failure patients after discharge from hospital, which includes several group workshops.
Unfortunately, these workshops are not always well attended by patients, who are not sufficiently aware of the seriousness of their disease and the changes it implies in their daily lives. 50% of patients relapse and are readmitted to hospital 6 months after discharge. It is therefore vital to reduce this figure.
The UTHop’IA project aims to raise patients’ awareness of the importance of therapeutic education from the moment of hospitalization for cardiac decompensation, in order to improve patient follow-up and avoid further hospitalization.
What is the UTHop’IA project?
One of the aims of the UTHop’IA project is to set up a therapeutic education program for patients hospitalized for a heart failure attack, using digital tools and artificial intelligence.
Thanks to this innovative program, hospitalized patients will be able to discover and assimilate “key” information to help them understand their illness: What treatments and new habits can you incorporate into your daily routine? How do I apply the salt-controlled diet? What are the warning signs of impending decompensation?
The UTHop’IA project, which will continue to develop for a few more years before it becomes available, aims to support patients from their hospitalization to their return home:
- While the patient is in hospital, information is delivered interactively by a humanoid robot,
- Once discharged from hospital and back at home, the patient’s awareness continues via a computer or smartphone, where he or she can find the same interface used during hospitalization. The artificial intelligence remembers previous interactions with the patient.
- In the weeks that follow, voice-mediated telemonitoring is set up (via computer or smartphone) to monitor the patient’s new disease-related habits.
An innovative project structured into 5 research sub-projects
The UTHop’IA project is structured into 5 research sub-projects to develop the various pedagogical and technical aspects of the therapeutic education program:
- ROB’EDUC: creation of a therapeutic education program (quizzes, advice, etc.). This sub-project benefited from the institutional support of AstraZeneca and the collaboration of students from the ECE engineering school. Find out more about the ROB’EDUC sub-project.
- ROBMAP: research into the autonomous navigation of the humanoid robot, called Charlie, within the hospital ward to visit patients, with the help of students from
- ROBARM: design of an automated arm for the Charlie robot’s autonomy in opening service doors, with the help of Polytech students in collaboration with Capgemini Engineering.
- CAP BOT VOCAL: development of a “voice bot” assistant using artificial intelligence, with the help of students from Pantheon Sorbonne University.
- CAP BOT DESIGN: development of a connected speaker to complement the existing tablet, with the help of students from Polytech Sorbonne.
They support the UTHop’IA project
The UTHop’IA project is led by Dr Françoise Pousset, Prof Richard Isnard and Dr Lise Legrand (IHU ICAN). “We are convinced that this highly innovative project will support the work of our medical teams. The Charlie robot will reinforce our teams, not to replace human contact, which is essential, but to free up more time for patient care and follow-up during hospitalization.
“This innovation will give medical teams a real break from the frenetic pace of care. The benefits will be felt not only by caregivers, but also by patients, who will be better equipped to deal with their illness. “Aurélie Foucher, Scientific Operations Manager on the UTHop’AI project.
For its ROB’EDUC sub-project, the UTHop’IA project benefited from the institutional support of AstraZeneca, as well as from the mobilization of IHU ICAN employees who raised funds during the 2022 Heroes’ Run.
ROB'EDUC: artificial intelligence at the service of therapeutic education
ROB’EDUC: artificial intelligence at the service of therapeutic education
The ROB’EDUC project, led by Prof. Richard Isnard, Dr. Françoise Pousset and Dr. Lise Legrand, aims to set up a therapeutic education program for patients hospitalized for a heart failure attack (HF), using artificial intelligence via a humanoid robot.
To carry out this project, IHU ICAN obtained institutional support from AstraZeneca to develop the design of the robot/patient interface and the creation of educational content for patients.
Learn more about this ambitious project below!
Therapeutic education: the key to heart failure treatment?

Like all chronic diseases, heart failure requires follow-up treatment throughout the patient’s life.
Despite advances in management, 1 in 2 patients die within 5 years of diagnosis.
It is therefore essential to accompany the patient and his entourage in the care process through therapeutic education, which plays a major role in the management of the disease:
- Improved compliance with treatment,
- Decrease in hospitalizations,
- Better quality of life.
Some background on heart failure (HF)
- A person has heart failure when his or her heart has difficulty pumping enough blood to oxygenate all the organs.
- 1.5 million people are affected in France, mainly but not exclusively people over 75 years old,
- Each year, 120,000 new cases are diagnosed, 200,000 hospitalizations and 70,000 deaths are due to CI,
- Possible causes: myocardial infarction, high blood pressure, diabetes, rhythm disorders such as atrial fibrillation, heart muscle diseases (cardiomyopathies) often of genetic origin and cardiotoxicity of certain drugs…
- Symptoms: abnormal shortness of breath on exertion, weight gain, edema, fatigue…
Providing therapeutic education: a challenge for medical teams
Since 2006, physicians in the cardiology department of the Pitié-Salpêtrière Hospital have set up a therapeutic education program (ETP) in heart failure after hospital discharge that includes several group workshops.
Unfortunately, less than 50% of the patients hospitalized in the cardiology department of the hospital can benefit from this program, partly because of the lack of medical and paramedical time of the staff trained to deliver it, and partly because of the low level of mobilization of patients to attend the workshops.
This is why, for many years, we have wanted to start therapeutic education as soon as patients are hospitalized for cardiac decompensation in order to make them aware of the importance of adopting new reflexes to improve their follow-up and avoid a new hospitalization.

Indeed, 50% of patients are rehospitalized 6 months after discharge. It is essential to reduce this number.
Moreover, in a context where telemedicine is increasingly developing, therapeutic education programs are still carried out in the traditional way in the form of workshops and paper brochures.
For several years, the cardiology department has been at the forefront in the implementation of remote monitoring, but the teams wish to go further in its use to better support patients.
The ROB’EDUC project: artificial intelligence for therapeutic education
To address this issue, IHU ICAN is currently developing the ROB’EDUC project, as part of the overall UTHopIA project.
The objective of the UTHopIA project is to use a humanoid robot to support the medical teams in delivering the Therapeutic Education Program (TEP) to patients hospitalized for a heart failure attack.
After clinical stabilization of the patient, the robot will be able to come and start the ETP program directly in the room of the hospitalized patient. It will have to interact with the patient by voice and through an interactive screen (tablet).
After the patient is discharged, interaction with the artificial intelligence can continue through a mobile application using the same interface with which the patient is already familiar. This application will keep track of the specific interaction that took place with each patient in order to personalize the follow-up.
The ROB’EDUC project seeks to prove the effectiveness of using digital media, robotics and artificial intelligence (AI) to improve patient compliance with therapeutic education programs.
What are the specific objectives of ROB’EDUC?
The ROB’EDUC project focuses on the digitization of therapeutic education content, the installation of elements in the robot system, the professionalization of user interaction and the development of design and navigation comfort.
The 3 TVE goals we want to achieve with the help of artificial intelligence and a humanoid robot are:
- To help the patient recognize the warning signs of decompensation that should lead to a consultation.
- Introduce patients to the salt-controlled diet and its importance.
- Learn to recognize the need for medical treatment and the importance of compliance.
This robot will answer the most common and useful questions to prevent a relapse.
This approach will engage the patient and may also have a ripple effect on caregivers to relay key messages.
The actors involved in the ROB’Educ project
- Dr Françoise Pousset, Cardiologist – Hospital Practitioner, Head of consultation and non-invasive platform, Heart Institute / IHU-ICAN
- Prof. Richard Isnard, University Professor – Hospital Practitioner, Head of the ARCHIMEDE medical-university department (cardiometabolism), Heart Institute / IHU-ICAN
- Dr Lise Legrand, Cardiologist – Hospital Practitioner, Heart Institute
- With the institutional support of AstraZeneca
This project has also benefited from the support of ICAN HCI employees and their families as part of the Race for Heroes 2022.
World Heart Day 2022: How to better detect atrial cardiomyopathy to avoid atrial fibrillation?
World Heart Day 2022: How to better detect atrial cardiomyopathy to avoid atrial fibrillation?
On World Heart Day, Thursday, September 29, 2022, it is important to remember that the atrial fibrillation or atrial fibrillation (AF) is the most common heart rhythm disorder. In France, it is estimated that it affects 750,000 people and that it is responsible for nearly 20% of ischemic strokes (obstruction of the cervical artery).
To fight against this cardiac disorder, the ICAN UHI is developing MAESTRIA, an innovative project that aims to better detect atrial cardiomyopathy, responsible for the occurrence of atrial fibrillation and vascular embolic accidents, thanks to a consortium of 18 international partners. Discover this ambitious project below!
Atrial fibrillation, a growing heart disease

Heart rhythm disorders often cause a sensation of abnormal heartbeat (palpitation, irregular heartbeat…), but they can also be asymptomatic and diagnosed during a heart examination. They represent the 1st cause of sudden death before 35 years.
A rapidly growing heart disease, atrial fibrillation is a heart rhythm disorder strongly linked to the aging population. Up to 8% of people over the age of 80 suffer from it, and 110,000 to 230,000 new cases appear each year. The increase in its incidence and prevalence results in an estimated cost of care of approximately 2.5 billion euros per year in France.
It is therefore essential today to better understand this pathology, a real economic and public health issue.
The MAESTRIA project, in response to this public health issue
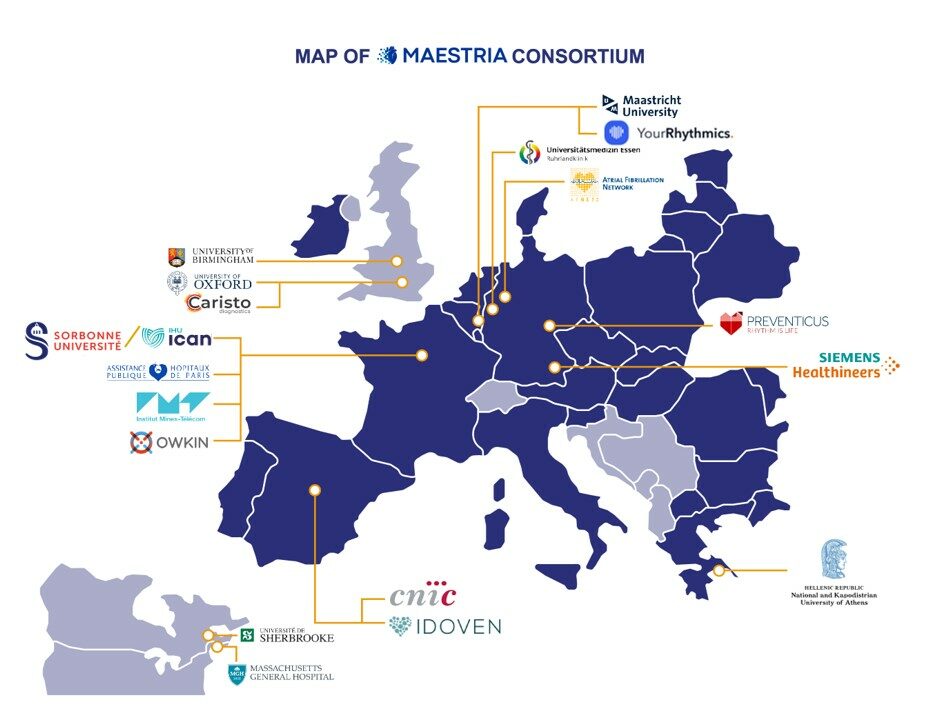
Launched in September 2021 and coordinated by Sorbonne University, the MAESTRIA (Machine Learning and Artificial Intelligence for Early Detection of Stroke and Atrial Fibrillation) research project has responded to the H2020 call for projects on digital diagnosis.
This international consortium brings together 18 partners from several European countries, the United States and Canada.
The objective of the project is to develop the 1rst digital platform for integrative diagnosis of atrial cardiomyopathy.
This tool will combine imaging data with physiological data (omics, clinical…) of patients, in order to obtain improved diagnostic accuracy through the identification of new therapeutic targets.
Its objective is to better prevent the complications of atrial cardiomyopathy (atrial fibrillation, strokes…) in order to increase the effectiveness and efficiency of treatments.
The project includes 3 strategic areas:
- Personalized diagnosis and innovative multidisciplinary care pathway, using genomic, metabolic and tissue inflammation research data,
- Risk stratification in AF patients with the use of artificial intelligence,
- Deployment of a digital diagnostic platform at the European level.

Who are the actors involved in this innovative project?
The 18 partners of the MAESTRIA consortium:
- Sorbonne Université (IHU ICAN)
- Assistance Publique des Hôpitaux de Paris (AP-HP)
- Oxford University
- Birmingham University
- AFNET
- Essen University
- Maastricht University
- National and Kapodistrian University of Athens
- CNIC
- Massachusetts General Hospital
- IMT Transfert
- Centre de Recherche du CHU de Sherbrooke
- Siemens Healthcare
- Caristo Diagnostics Limited
- Owkin
- Idoven
- Preventicus
- YourRhythmics
IHU ICAN obtains a €1.5M grant for its Heart & Aorta Atlas!
Heart-Aorta Atlas project: €1.5M grant from the France 2030 plan
With the Heart and Aorta Atlas project, the ICAN IHU aims to create a reference Atlas of human 4D cardiac imaging with strong industrial appeal, to fill an information gap on a national scale.
The objective of this project is to help economic players in the medical imaging, pharmaceutical, medical device and digital simulation industries to design new approaches for cardiovascular health.
Promoted by INSERM, the project is supported by the French government and the Ile-de-France region through a 1.5 million euro grant obtained as part of the “SESAME Filières” France 2030 call for projects.

SESAME aid, support for scientific competitiveness in Paris Region
To strengthen the skills of the Ile-de-France scientific ecosystem, the Ile-de-France region is setting up the SESAME “Scientific and Technological Facilities and Platforms” program, which is part of the regionalized Avenir Investment Program (SESAME filière PIA).
- The objective: supporting the development of research laboratories through innovative projects and original experimental devices, in order to structure centers of scientific excellence in Île-de-France,
- Beneficiaries:non-profit research or higher education institutions (public or private) located in the Paris Region.
Within the framework of this call for projects “SESAME Filières”, the IHU ICAN obtained a grant of 1.5 million euros for the creation of an interoperable and multidisciplinary infrastructure in hemodynamic cardiovascular imaging with strong industrial appeal: the Heart Aorta Atlas.

The Heart & Aorta Atlas project, a response to an urgent need for knowledge
Numerous data converge today to make us aware that the mechanisms of aging, pathophysiological, cardiovascular and metabolic begin earlier in life than previously anticipated. From the age of 40 onwards, certain degenerative, oncogenic and inflammatory processes begin to manifest themselves.
Medical imaging has a key role in the detection, evaluation, and management of patients, but the study of these subclinical multi-organ alterations is very limited. Indeed, most large international cohorts recruit subjects over this age.
To address this urgent issue, the ICAN UHI plans to create a large biomedical imaging database linked to the national cohort CONSTANCES (INSERM).
What are the objectives of the Heart Aorta Atlas project?
The imaging data collected will be unique in that it will combine analysis of the structure and function of the heart, vessels and liver at a scale not currently available and through non-invasive examinations.
The main objectives are to:
- To establish the values of new imaging biomarkers in an asymptomatic French population according to sex, age and risk profile based on existing data in the CONSTANCES cohort,
- Understanding the origin of diseases and their early detection at a sub-clinical stage, the determination of new individual cardiovascular and metabolic risk profiles, the constitution of a reference multimodal imaging cohort for research on frequent and rare diseases.

What assets for the industrial ecosystem?
Thanks to this work, the Heart-Aorta Atlas project will have a strong added value for the industrial ecosystem, by offering :
- The creation of a unique pole of partnership excellence in Ile-de-France, around a structured and interoperable bank of labelled images, software and validated cardiovascular biomarkers,
- The availability of advanced imaging including anatomical, functional but also hemodynamic evaluation of the heart and aorta in population.
This catalog of expert imaging data will integrate raw images, post-processed images, quantitative measurements and medical readings, complemented by analysis software.
The service offer(clinical validation, software test benches, medical device design assistance, digital twins…) is aimed at manufacturers in the following economic sectors:
- Pharmaceutical industry,
- Medical imaging industry,
- Medical devices sector,
- Digital simulation sector,
The actors involved in the Heart-Aorta Atlas project
Grâce à ses liens avec des pôles de compétitivité comme Medicen et Cap Digital, le projet Atlas Cœur Aorte est porteur d’une empreinte territoriale forte.
Au niveau de l’expertise scientifique, il implique l’excellence des acteurs suivants :
- Pr Alban REDHEUIL, porteur du projet, Professeur des Universités – Praticien des Hôpitaux. Cardioradiologue, Responsable de l’imagerie cardiovasculaire et thoracique ICT Hôpital Pitié-Salpêtrière, APHP.SU, Responsable médical du plateau de recherche imagerie de la Fondation pour l’Innovation en Cardiométabolisme et Nutrition (IHU ICAN)
- Mme Nadjia KACHENOURA, DR Laboratoire d’Imagerie Biomédicale INSERM/CNRS/SU/IHU ICAN
- Mme Khaoula BOUAZIZI, IR LIB Imaging IHU ICAN
- Mme Louise MEYFROIT, Chef de projet dédié Imagerie IHU ICAN
- Pr Ariel COHEN, Service de Cardiologie, Hôpital Saint Antoine, APHP, Sorbonne Université IHU ICAN
- Dr Laurie SOULAT-DUFOUR, Service de Cardiologie, Hôpital Saint Antoine, APHP, Sorbonne Université IHU ICAN



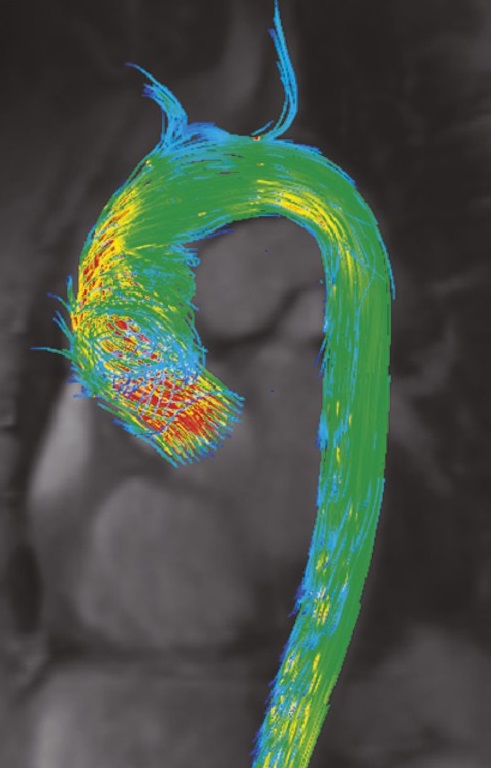
Projet CMRAI : Detecting the vulnerable aorta in MRI for precision cardiovascular medicine
CMRai project: Detecting the vulnerable aorta in MRI for precision cardiovascular medicine
The aortic aneurysm is a permanent dilation of the aorta whose consequences, in the event of rupture, can be fatal. If diagnosed early enough, treatment often relies on managing high blood pressure. In other cases, surgery is considered to treat the aneurysm as soon as possible. But unfortunately the diagnosis is often late, made during the rupture, and constitutes a dramatic event associated with a mortality rate of 80-90%. It is in this context that it is necessary to better detect aortic aneurysms in the French population. So how can we better prevent aortic ruptures? This is the challenge taken up by the CMRAI project led by the IHU-ICAN and Sorbonne University and funded by EIT Health.
This project, set up at the initiative of the IHU-ICAN and coordinated by its founder Sorbonne University, brings together 9 European partners: Assistance Publique-Hôpitaux de Paris (France), the Hanover School of Medicine (Germany), the Medical University of Vienna (Austria), Vall d’Hebron Hospital (Spain), Santa Cruz Hospital (Portugal), Lisbon University of Sciences (Portugal), including 2 industrial partners: Imageens (France ) and Siemens Healthineers (Germany).
The objective of the CMRAI project is to create a platform that will make it possible to define, from the first signs of the disease, an aortic aneurysm risk score for each patient, and therefore to define a personalized follow-up and management strategy.
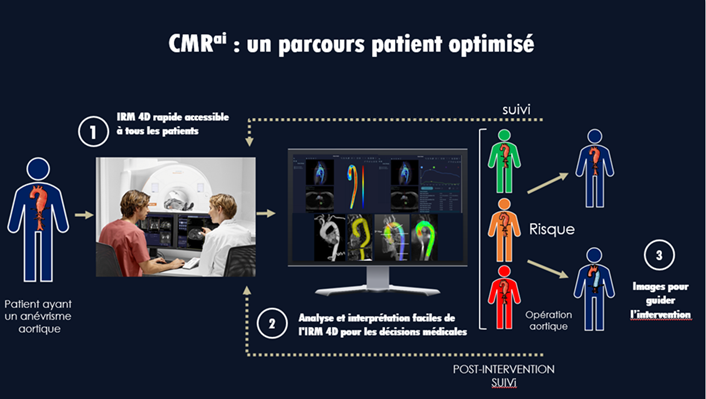
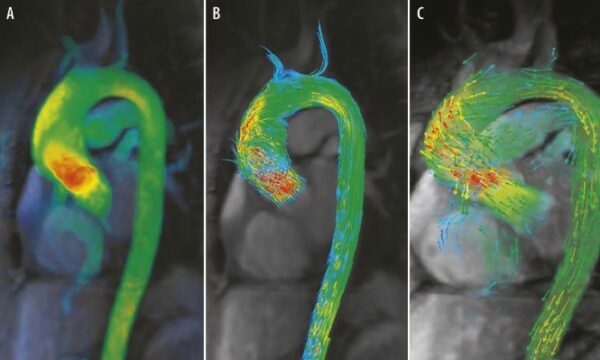
This project proposes to go beyond the practice based on diameter alone by proposing an evaluation of new functional parameters in MRI accounting for the elasticity of the wall of the aortic aneurysm, the shear forces applied to its wall, the pressure regime and the disturbances of the resulting blood flows.
These innovative parameters from algorithms developed by the LIB biomedical imaging laboratory (Inserm/SU/CNRS) will be studied in two populations: in patients with a thoracic aortic aneurysm as part of a clinical study in 5 European reference centers and in healthy subjects recruited from the Constances cohort (Inserm) in France in order to establish the normal values expected in the general population.
Led by Prof. Alban Redheuil, head of Cardiovascular and Thoracic Imaging (ICT) at Pitié-Salpêtrière hospital and medical manager of the ICAN Imaging platform, by Dr Nadjia Kachenoura, head of the cardiovascular imaging team ( iCV) of the Biomedical Imaging Laboratory (LIB) and by Ted Baldwin CEO of the start-up Imageens, the CMR projectAI involves several departments of the IHU-ICAN:
- The Scientific Operations Service(SOS) for setting up the project, monitoring the clinical study and scientific coordination
- The Clinical Investigation Platform for the management of clinical study patients
- The ICAN Imaging Platform for the acquisition of 550 MRI scans of the Parisian participants of the clinical study
Expected results
CMRAI will therefore allow the screening of the aortic aneurysm, the therapeutic decision-making and the adapted and personalized care thanks to Magnetic Resonance Imaging (MRI) coupled with the automated and multiparametric analysis of the aorta.
This study contributes to the development of precision medicine in cardiometabolic diseases. This is a major project that has obtained EIT Health funding.

April 7, 2022: World Health Day: The IHU model to tackle the public health challenge of cardiometabolic diseases and accelerate medical innovation at the service of the patient.
World Health Day: The IHU model to tackle the public health challenge of cardiometabolic diseases and accelerate medical innovation at the service of the patient.
Created in 2011, the IHU ICAN (Foundation for Innovation in Cardiometabolism and Nutrition) is a center of excellence in the field of metabolic diseases: diabetes, obesity, liver diseases (steatosis), heart and vessel diseases. These pathologies represent the first cause of chronic diseases. So how does the “IHU” model make it possible to fight effectively against this scourge?
1- With teams of experts
The strength of the IHU model lies in the concentration of significant human resources on targeted public health priorities, supported by agile structures, and in bringing together clinicians, researchers and entrepreneurs in the service of patients.
IHUs represent a force for innovating and developing the paths, treatments and medical devices of tomorrow. ICAN teams accelerate discoveries on metabolic diseases and their transfer to the benefit of patients thanks to integrated procedures that demonstrate responsiveness and agility from project set-up to the valorization of the discovery.
2- With the decompartmentalization of disciplines.
Changing scale to invent the medicine of tomorrow in cardiometabolism.
Cardiovascular diseases related to diabetes, atherosclerosis, obesity or liver diseases such as NASH are grouped under the concept of cardiometabolic diseases. There are scientific bases for this concept of cardiometabolic diseases consisting of the many interfaces between metabolism and organs: microbiota, adipose tissue, immune system. Thus, we have moved from a medicine centered on an organ to a global and systemic approach to cardiometabolic diseases.
The management of patients with metabolic diseases is modified, doctors no longer reason by organ or by disease but they implement a personalized and multidisciplinary approach for a global management of the disease and its consequences on the future. patients.
For example, not all obese patients develop diabetes or serious cardiovascular pathologies, just as not all diabetic patients have heart failure. Conversely, some individuals a priori at low risk will have a myocardial infarction. It is therefore necessary to better understand the interactions between the organs and between the pathologies in order to better manage the patients and anticipate the evolutions. It is necessary to determine which patient will develop which syndrome.
New causal relationships have emerged. “NASH (non-alcoholic fatty liver disease), for example, which until then was considered an indicator of malnutrition and systemic disease, turns out to be much more than that: it has a direct impact on the vessels, the microbiota, the tissue fat and overall metabolism ». Pr Stéphane Hatem, Director of ICAN
The organs dialogue with each other, and when one of them begins to suffer from metabolic disturbances, the messages sent can domino and trigger deleterious processes at a distance.

Developing knowledge of pathophysiological links, identifying biomarkers and evaluating them in populations are key steps in understanding metabolic diseases. To do this, the IHU ICAN participates in innovative research programs on integrating the use of health data generated by new imaging or research techniques thanks in particular to the explosion of omics in health. Much work remains to be done, but advances in biology and new technologies are accelerating research innovations. Entirely dedicated to the study and understanding of metabolic diseases, the IHU ICAN is a pioneer in research on cardiometabolism.
Some examples of innovative projects for patient services carried out by the IHU ICAN:
Successful launch of the XVIVO trial
Successful launch of the XVIVO trial
Launch of the pre-CE marking industrial trial conducted by XVIVO Perfusion, in collaboration with Dr Guillaume Lebreton, thoracic surgeon in the cardio-thoracic surgery department headed by Pr Leprince, aimed at validating the performance of a new system for transporting grafts intended for heart transplantation.
This innovative method of protecting the grafts involves connecting the heart, of the donor cooled at rest, to a pump which administers a preservation solution, oxygen and nutrients throughout the duration of the transport. Unlike the standard transport method, which simply involves placing the heart in a chilled liquid, this new solution will better meet the nutritional needs of the heart and allow to increase the chances of success of the transplant, especially when the heart has to travel a long way to reach the recipient.
The Pitié-Salpêtrière site 1st recruiting center for this trial
Thanks to the joint work of the Scientific Operations teams for setting up the project and the ICAN clinical investigation platform, the Pitié-Salpêtrière hospital is the first recruiting center for this trial with 11 patients in 6 months on the 30 planned in total. Currently, 11 hospitals are involved in this innovative project. The total duration of the study is 2 years. »