Heart failure is a frequent and serious chronic disease that affects more than 1.5 million people in France. Every year :
- 120,000 new cases are diagnosed
- 165,000 people are hospitalised due to cardiac decompensation
- 70,000 people die from the disease
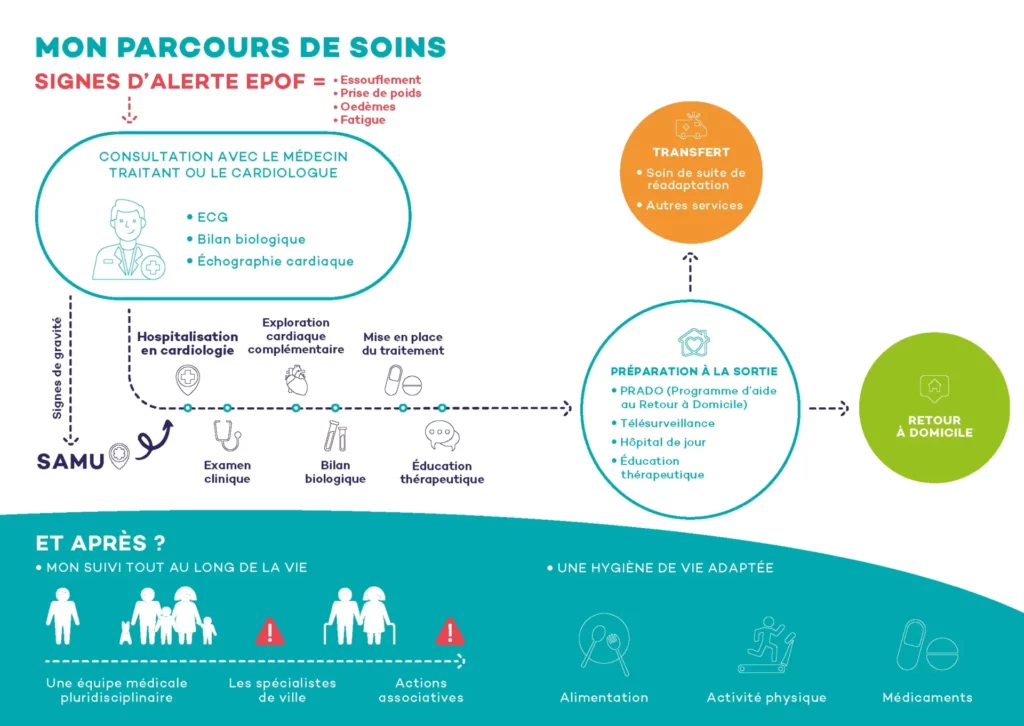
50% of patients will be readmitted to hospital 6 months after discharge for cardiac decompensation. An effective care pathway needs to be put in place, involving the patient and medical and paramedical healthcare professionals in the community and in hospital. The aim is toimprove patient follow-up after hospitalisation, and to detect and manage cardiac decompensation early, in order to reduce relapses and the number of patients returning to hospital in emergency conditions. What treatment is available today for heart failure?
Care and treatment of heart failure
1- Diagnosis
Heart failure occurs when the heart has difficulty pumping enough blood to oxygenate all the organs. It may be the result of a myocardial infarction, high blood pressure, rhythm disorders (atrial fibrillation) or heart muscle disease (cardiomyopathies), often genetic in origin.
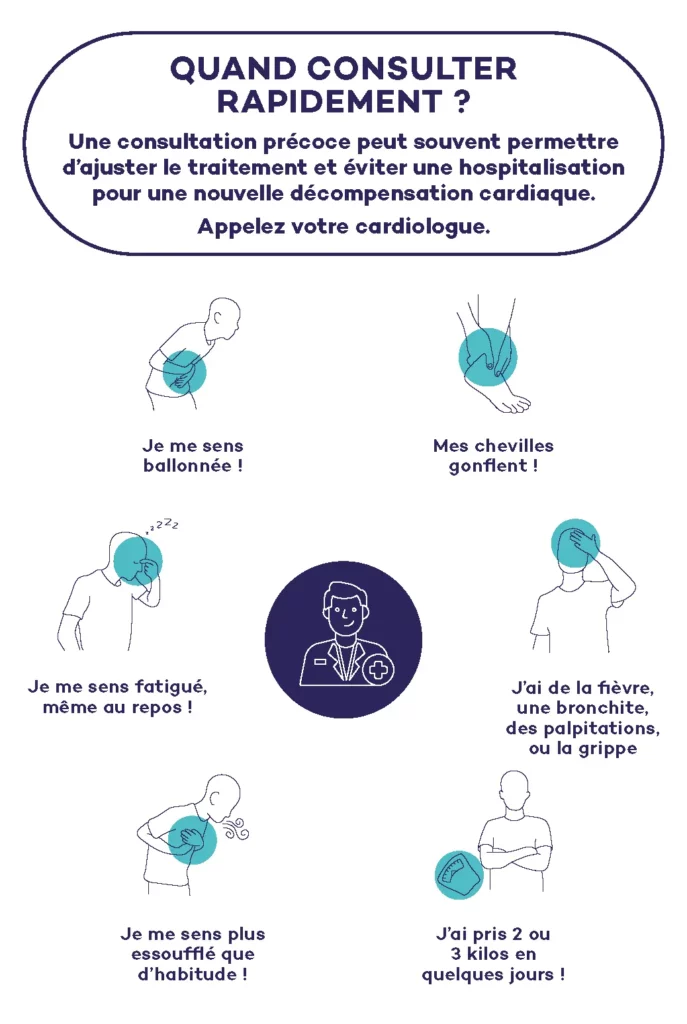
The main symptomsare abnormal breathlessness on exertion, weight gain, oedema and unexplained fatigue. In the presence of these symptoms, a medical consultation is necessary in order to make a diagnosis, based on the measurement of natriuretic peptides and echocardiography, and to begin treatment.
This is usually done by a general practitioner or cardiologist, but if there are signs of seriousness, the diagnosis will be made in an emergency department. Early treatment can slow the progression of the disease and prevent serious cardiac decompensation.
2- Initial assessment
A number of tests are carried out to assess the severity of theheart failure (HF), find its cause and identify any associated pathologies:
- Clinical examination,
- Complementary examinations such as cardiac ultrasound, chest X-ray, blood test for biological assessment and measurement of cardiac biomarkers (NtproBNP),
- Search for comorbidities.
The various results will help guide the treatment and specify the patient’s follow-up arrangements.
This phase will also enable us to determine with the patient:
- The impact of heart failure on activities of daily living,
- The problems posed by associated co-morbidities,
- Their expectations and motivations for change,
- Their ability to modify their lifestyle,
- Any barriers to effective management (psychological and social),
- For elderly patients (>75 years old): an additional assessment of their cognitive functions, autonomy and nutritional status may be necessary.
3- Treatment of heart failure, follow-up and therapeutic education
The aim of treatment is to prevent episodes of decompensation, reduce the number and length of hospitalisations, and slow the progression of the disease by reducing the risk of mortality. Another aim of treatment is to improve patients’ quality of life by alleviating their symptoms (breathlessness, fatigue, oedema, etc.) so that they can live better every day.
The management of heart failure is therefore comprehensive, and treatment always includes :
- Non-pharmacological treatment: new eating habits (low-salt diet) and regular exercise,
- Pharmacological treatment,
- And, in some cases, an electrical device: bi-ventricular pacemaker, implantable defibrillator, etc

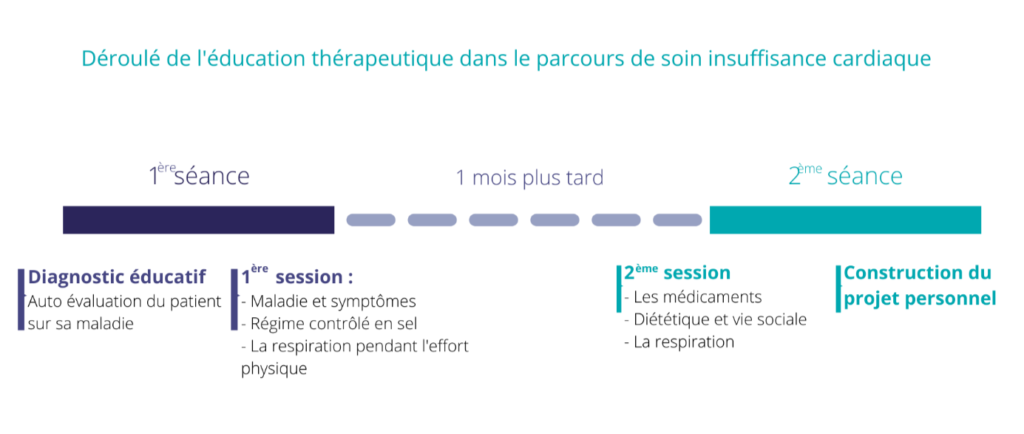
Since 2006, doctors at the Pitié-Salpêtrière Heart Institute and the ICAN have been working with the department’s nurses and dieticians to set up a therapeutic education programme (ETP) for heart failure. It is an integral part of the patient’s care pathway.
Offered to patients shortly after diagnosis, the programme comprises several group workshops (programme 10/326 accredited by the ARS). The aim of therapeutic education is to help patients (and those around them) acquire the skills they need to manage their disease, make it more manageable and prevent avoidable complications.
The cardiology department and the ICAN IHU have set up 6 workshops, each lasting 1 hour, covering a number of key topics: the disease and its symptoms, nutrition and physical activity. In practice, patients come for 2 days of outpatient treatment, 1 month apart.
- Day 1 : an educational diagnosis is carried out by the team with the patient to find out his or her level of knowledge about his or her disease and his or her expectations of the EPT programme offered. Once this self-test has been carried out, a multidisciplinary medical team proposes and organises a therapeutic education programme with the patient, based on the nature of their skills and the stage and progress of their disease. The day continues with the patient taking part in 3 workshops: on the pathology (its symptoms and the signs that should lead them to consult a doctor when they occur), on a salt-controlled diet and on breathing during physical effort so as to practise regular physical activity comfortably.
- 1 month later: a second day of therapeutic education is scheduled with the patient to complete and finalise the programme by taking part in the final workshops on medication, diet and its compatibility with social life, as well as a more in-depth look at breath management during exercise. This second day is an opportunity to work with the therapeutic education team to develop a personal project for the patient.
This programme is enriched over the years to adapt to new medical and paramedical practices and patient behaviour. The integration of digital tools from the time of hospitalisation is currently being evaluated, to make more patients aware of the risks associated with their disease and the solutions available to help them better manage their CI.
- Day 1 : an educational diagnosis is carried out by the team with the patient to determine their level of knowledge about their disease and their expectations of the EPT programme offered. Once this self-test has been carried out, a multidisciplinary medical team proposes and organises a therapeutic education programme with the patient, based on the nature of their skills and the stage and progress of their disease. The day continues with the patient taking part in 3 workshops: on the pathology (its symptoms and the signs that should lead them to consult a doctor when they occur), on a salt-controlled diet and on breathing during physical effort so as to practise regular physical activity comfortably.
- 1 month later: a second day of therapeutic education is scheduled with the patient to complete and finalise the programme by taking part in the final workshops on medication, diet and its compatibility with social life, as well as a more in-depth look at breath management during exercise. This second day is an opportunity to work with the therapeutic education team to develop a personal project for the patient.
This programme is enriched over the years to adapt to new medical and paramedical practices and patient behaviour. The integration of digital tools from the time of hospitalisation is currently being evaluated, to make more patients aware of the risks associated with their disease and the solutions available to help them better manage their CI.

4- The return home: a key stage in the progression of the disease
In the event of hospitalisation, the care pathway should enable patients to be prepared for discharge from hospital, to ensure continuity of care in the community under the best possible conditions, especially if the disease is discovered. The majority of patients who return home after hospitalisation often feel left to their own devices, with insufficient information about their illness and what to do if it worsens.
At present, patients are given a hospital discharge report and this is sent to their referring doctors. For practical reasons (availability, waiting times, lack of understanding), the majority of patients with heart failure cannot see their GP or cardiologist until around 6 weeks after discharge. This delay makes it difficult to monitor post-hospitalisation and optimise drug treatments, whose dosage must be gradually increased.
To improve monitoring of patients after discharge from hospital, remote monitoring programmes have been set up by the health insurance scheme.
- Programme d’aide au retour à domicile (PRADO): several home visits by a nurse as soon as the patient returns home for monitoring and therapeutic education, as well as organising appointments with the GP and cardiologist, are managed by dedicated staff prior to the patient’s discharge, and a monitoring booklet is given to the patient.
- Another remote monitoring option that can complement PRADO is remote monitoring of heart failure, developed as part of the ETAPES programme (Experimentation de télémédecine pour l’amélioration des parcours en santé). Using a tablet and a connected scale delivered to the patient’s home, the patient transmits his or her symptoms and weight to a platform that filters alerts and forwards relevant alerts to the remote monitoring centre (in this case, the cardiology department at the Pitié-Salpêtrière hospital). This remote monitoring, which already exists for patients fitted with defibrillators or pacemakers, enables patients to be monitored more effectively and symptoms to be treated as soon as they appear, adapting treatment early when necessary in order to reduce the number of repeat hospitalisations and emergency room visits. After a trial phase, the Social Security Financing Bill has brought remote monitoring into the mainstream.
These new telemonitoring techniques and the importance of the possibility of early consultations to better monitor patients with heart failure and optimise their treatment have reinforced the need for teamwork. In the cardiology department at the Pitié Salpêtrière Hospital, the nurses (some of whom are under a cooperation protocol) manage the alerts from the remote monitoring service on a daily basis, in collaboration with the patients’ referring doctors. The nurse with the cooperation protocol also carries out heart failure treatment titration consultations, enabling the patient to be seen more regularly.
The care pathway for patients with heart failure has therefore evolved in recent years. It has been enriched while always trying to leave the patient at the centre of his or her care. Within this care pathway, communication between the various professionals involved in the patient’s care is vital, but must be constantly improved to ensure that it runs more smoothly. The new connected tools will undoubtedly help to achieve this.