Non-alcoholic fatty liver disease (NAFLD) is a chronic liver disease affecting around 25% of the population in Western countries. MAFLD is a continuum of pathological states ranging from simple steatosis to non-alcoholic fatty liver disease (MASH, formerly NASH), which may progress to fibrosis and cirrhosis and may lead to liver transplantation.
Metabolic steatopathy is defined by the presence of steatosis (accumulation of intrahepatic fat) in the presence of metabolic risk factors and in the absence of secondary causes of steatosis (excessive alcohol consumption of more than 20g/day for women and 30g/day for men, use of medication, etc). It may coexist with other causes of chronic liver disease (e.g. viral hepatitis, etc.).
Key figures for fatty liver (MASH)
Ref. Serfaty Gastroenterology 2020, CONSTANCES cohort
of the adult population in France affected by MAFLD
of the adult population worldwide affected by MAFLD
of the adult population in the United States affected by MAFLD
new cases of MASH in France in 2016
new cases of MASH in Europe in 2016
Average age at onset of MASH, mainly in men
deaths / year in France due to MASH
deaths / year in Europe due to MASH
deaths / year in the United States due to MASH
What are the symptoms?
Hepatic steatosis (MASH) is a silent disease. It is most often diagnosed by chance.
What are the warning signs of MASH?
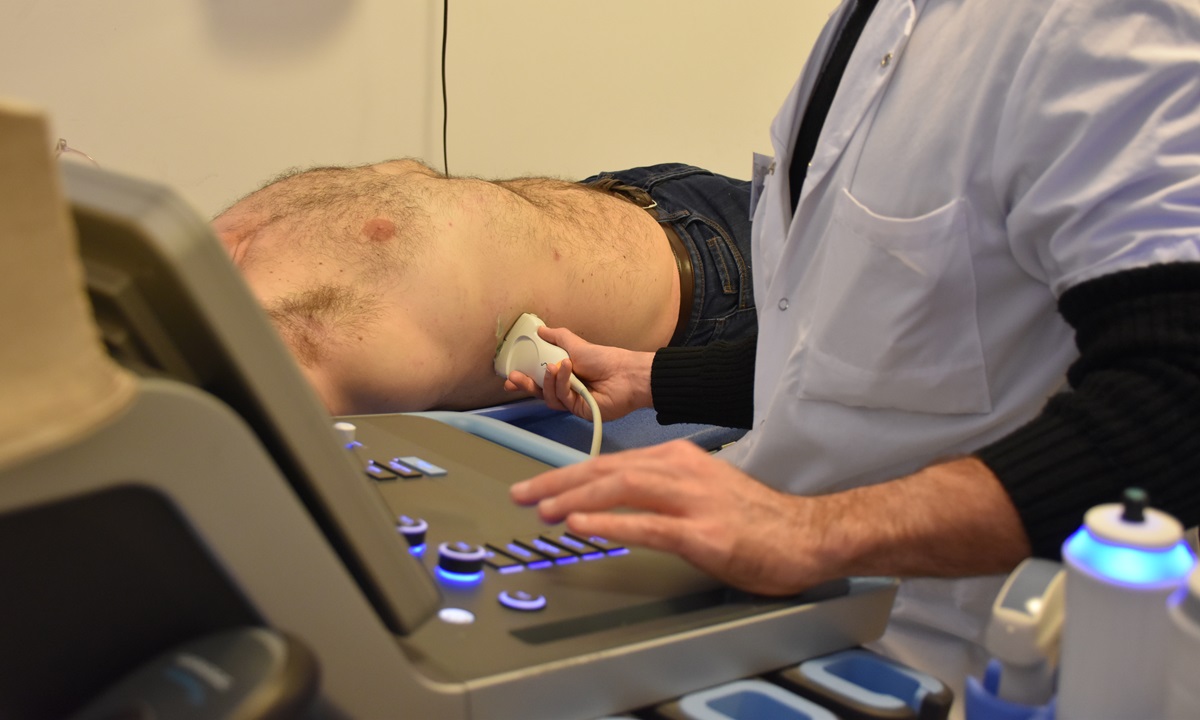
- Steatosis visible on ultrasound in the presence of metabolic risk factors
- Increased transaminases and steatosis on ultrasound
- Increased transaminases and metabolic risk factors
- Hyperferritinaemia associated with metabolic risk factors
- Sometimes diagnosed at the stage of cirrhosis
The spectrum of severity
- Isolated steatosis: accumulation of intrahepatic fat involving > 5% of hepatocytes
- Steatohepatitis (MASH, formerly NASH): accumulation of intrahepatic fat associated with necroinflammation, with or without fibrosis
- Cirrhosis: 15% to 30% of patients with NASH
- Decompensated cirrhosis, hepatocellular carcinoma and liver transplantation
What are the risk factors?
Closely related to insulin resistance and metabolic risk factors, the most important of which are as follows:
- Obesity (particularly visceral obesity – waist circumference > 102/88 cm men/women)
- Type 2 diabetes (steatosis is present in >70% of diabetic patients; diabetes is an established risk factor for fibrosis progression)
- Hypertension
- Dyslipidaemia
- Sleep apnoea
- Ageing
- Genetic (PNPLA3, TM6SF2) and epigeneticfactors (cases of familial aggregation in relation to environmental and epigenetic factors)
The risk of MAFLD increases in the presence of several risk factors (e.g. prevalence of steatosis > 91% in the presence of diabetes and obesity.

The course and consequences of MASH
- Patients with isolated steatosis progress little or not at all, and have a mortality rate comparable to that of the general population.
- Patients with MASH are at risk of disease progression: fibrosis progresses by approximately 1 stage every 7 years; cirrhosis (15% to 30% of patients with NASH); hepatocellular carcinoma; liver transplantation (currently the 2nd leading cause of liver transplantation in the US).
- Overall mortality increases with the severity of liver damage, becoming higher than in the general population from stage 2 fibrosis onwards.
- Liver-related mortality is the leading cause of death in cirrhotic patients (a 2 to 3-fold increase compared with the general population in the case of compensated cirrhosis, and a >10-fold increase compared with the general population in the case of decompensated cirrhosis).
- In non-cirrhotic patients, the leading cause of death is cardiovascular disease and extrahepatic cancers.

How is hepatic steatosis treated?
Hygienic dietary measures (diet, exercise) and optimal control of risk factors, particularly diabetes and weight loss, are strongly recommended for all patients, regardless of the severity of liver damage.
For obese patients, bariatric surgery can significantly improve liver damage in patients without advanced fibrosis. However, the results of bariatric surgery are more modest in cirrhotic patients or those with advanced fibrosis (≥ F3).
There is currently no effective approved treatment for MASH. Only dynamic and innovative research will improve patient care.
The ICAN IHU’s response: the MASH clinic
Teams from the AP-HP and ICAN have created the MASH clinic to offer patients an innovative, multidisciplinary and personalised care pathway. The aim of this pathway is to anticipate and intercept the complications of NASH (early atherosclerosis, high blood pressure, diabetes, etc.) and to offer personalised care to each patient.
The MASH clinic is the leading hospital-based facility for the diagnosis and multidisciplinary management of patients with metabolic steatosis in France.
NASH-related research
The IHU-ICAN teams are collaborating on several MASH research projects, including :
- EPOS / LITMUS
- HOTSURFER
- CORONASH for natural history and diagnostic tools
- EU-PEARL for treatment