Bariatric surgery
In 2017, around 68,000 people underwent bariatric surgery (bypass, sleeve or gastric band) to treat the most severe cases of obesity. According to a study by the Directorate for Research, Studies, Evaluation and Statistics (DREES), this figure has multiplied by 4.5 in ten years (15,000 patients operated on in 2006) and by more than twenty in twenty years (2,800 in 1997).
Obesity is a chronic disease and, particularly when it is severe or massive, can lead to difficulties in everyday life. It can also threaten health andcause chronic metabolic diseases such as diabetes, arterial hypertension, dyslipidaemia, dysmetabolic steatopathy, sleep apnoea syndrome, etc. These diseases are chronic diseases that progress to other pathologies such as cardiovascular disease.
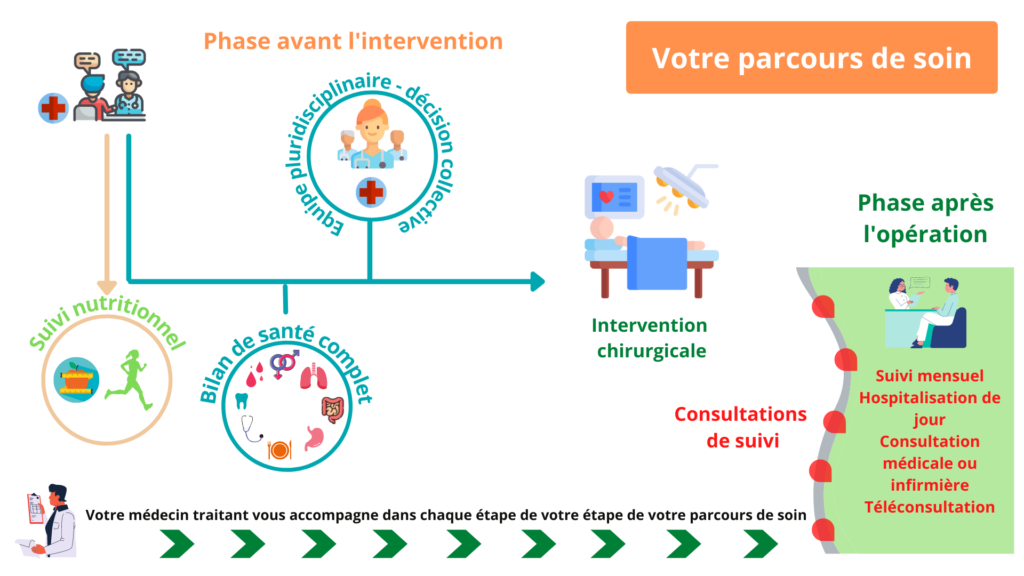

Bariatric surgery care pathway
Bariatric surgery leads to major and lasting weight loss, an improvement in the chronic pathologies associated with obesity, and an improvement in life expectancy and quality of life. It also reduces the incidence of chronic diseases associated with obesity. Nevertheless, undergoing surgery is an important decision, and requires careful preparation in compliance with national indications and contraindications, as well as lifelong care.
Doctors in the Nutrition Department at the Pitié-Salpêtrière Hospital are involved in writing and updating recommendations for the Haute Autorité de Santé on the management of patients suffering from severe obesity (including bariatric surgery).
It is therefore essential to provide adequate multidisciplinary preparation for this operation, and to be able to guarantee lifelong follow-up for these patients. Indeed, managing bariatric surgery is an ongoing process, which involves informing, assessing and supporting patients throughout their journey.
Patients undergoing bariatric surgery are cared for by multidisciplinary teams (doctors, surgeons, anaesthetists, nurses, dieticians, psychologists, physical activity instructors and a coordinator), in liaison with the treating doctor. This care is part of a personalised project for the patient, as described in the figure below.
1- Patient information and assessment
The first appointment is used to find out and assess whether patients meet the criteria for indications and contraindications for bariatric surgery, to ensure that care is appropriate. A day hospital is organised at the start of the programme to assess and inform patients, and to offer them a personalised preparatory programme so that they can make an informed and reasoned decision.
This discussion covers
- The different surgical techniques: their principles, benefits, risks and disadvantages, and the limits of surgery,
- The need to modify eating habits and lifestyle (regular physical activity) before and after the operation,
- The need for lifelong medical and surgical follow-up and the potentially serious consequences of failing to do so,
- The possibility of recourse to reconstructive surgery after bariatric surgery.
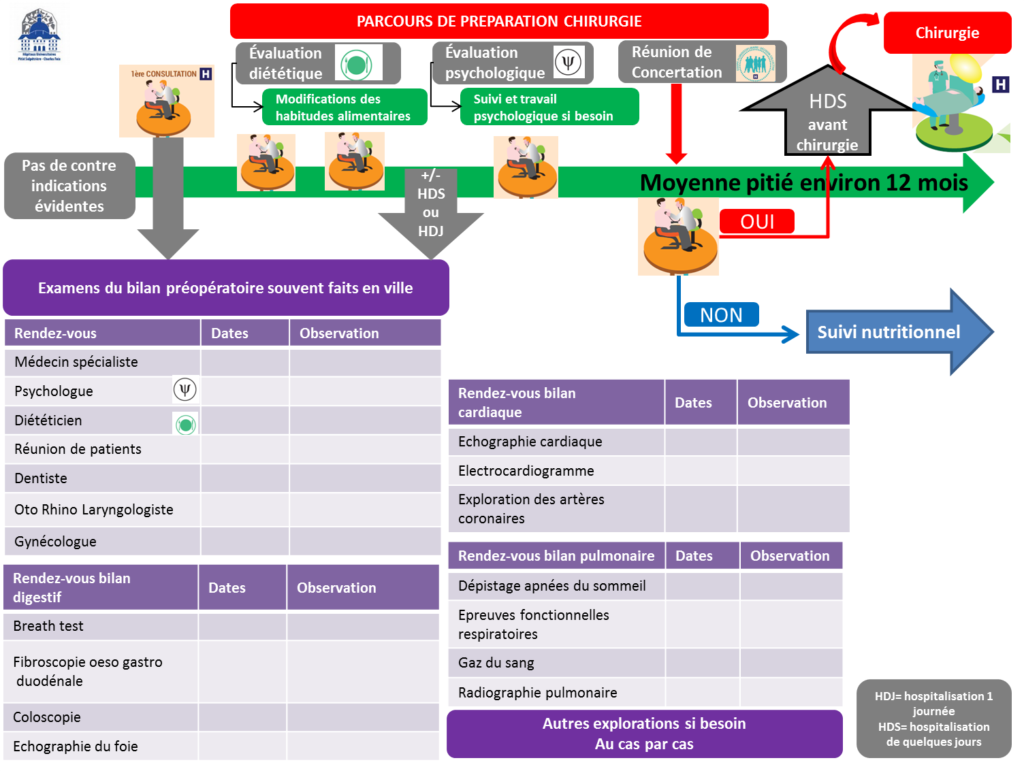

2- Assessing and managing the patient before the operation
A medical, surgical , dietary and psychological assessment must be carried out to limit the risks of surgery and ensure the long-term success of the operation.
This preoperative medical and surgical assessment includes in particular :
- An assessment and management of co-morbidities (cardiovascular, metabolic, respiratory, etc.),
- An assessment of eating behaviour and management of any eating disorders,
- A nutritional and vitamin assessment and correction of any deficiencies, and an assessment of chewing ability,
- The introduction of a therapeutic education programme covering diet and physical activity is recommended from the pre-operative period,
- Psychological and psychiatric assessment.
This is an essential stage, because following these examinations, the multidisciplinary team will discuss and agree whether or not to operate on the patient. As our department specialises in severe, complex and even rare cases of obesity, patient files sometimes have to be discussed several times in order to analyse and establish the best diagnostic and therapeutic strategies.
3- Post-operative follow-up
Because obesity is a chronic disease, and because of the risk of late complications (surgical or nutritional, some of which may lead to serious neurological damage), patients must be monitored and cared for after the operation for the rest of their lives.
- Follow-up is closer in the first year, with a consultation plan and a day hospital scheduled at 3 and 12 months.
- Thereafter, the patient will be monitored on an annual basis, with the exception of an outpatient hospital visit every 5 years to review the medical, nutritional and dietary situation.
A bariatric surgery care pathway dedicated to adolescents suffering from obesity is offered by ICAN specialists to meet their specific needs.

Patient information
Bariatric surgery
Booklet n°1
Bariatric surgery
ADULT
Booklet n°2
Bariatric Surgery
ADULT
Booklet n°3
Bariatric surgery
TEEN
Booklet n°4
Bariatric surgery
ADOLESCENT
Summary of good dietary practice
Bariatric surgery
ADULT
Summary of good dietary practice
Bariatric surgery
ADULT
Useful links
- Collectif national des associations d’obèses: https: //www.facebook.com/CNAObesite/
- Nutrition department: https: //www.aphp.fr/service/service-59-066
- French Association for Study and Research on Obesity: http: //www.afero.fr/